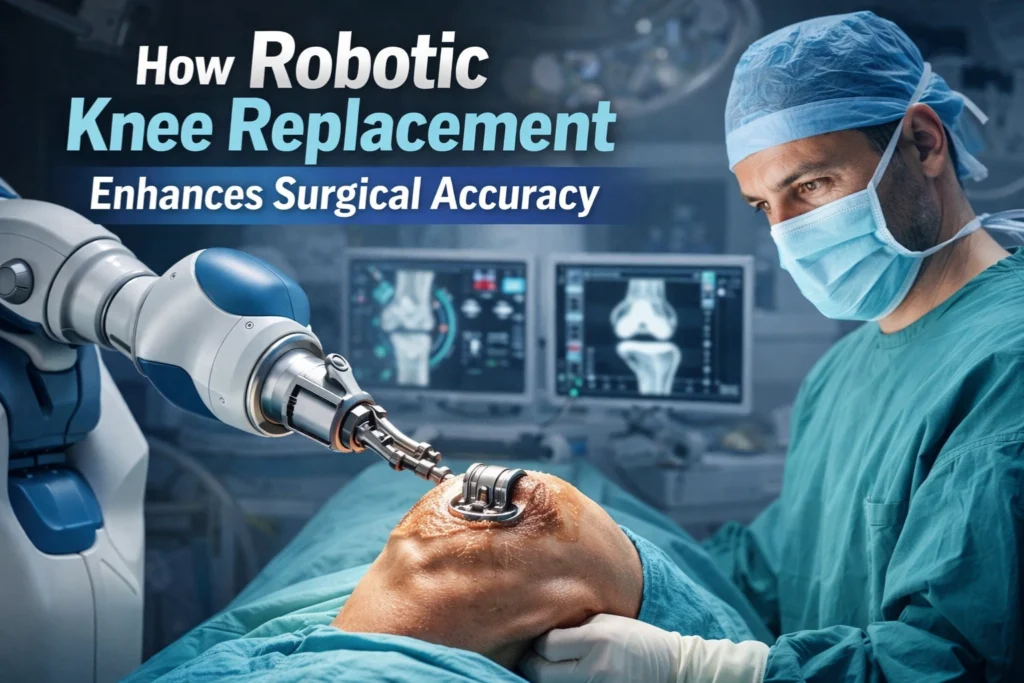
How Robotic Knee Replacement Enhances Surgical Accuracy & Precision
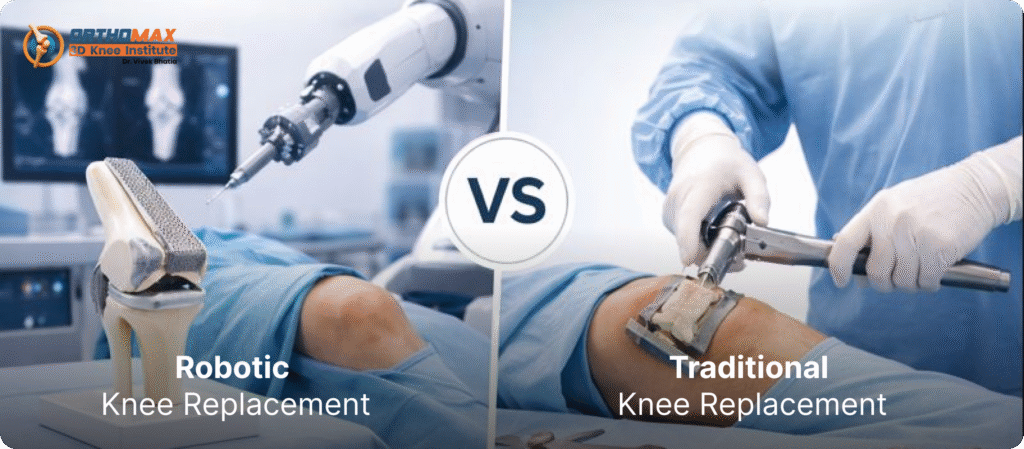
How Robotic Knee Replacement Enhances Surgical Accuracy & Precision Knee replacement surgery has evolved rapidly over the last decade. What was once a procedure driven largely by the surgeon’s experience and manual instruments is now guided by advanced technology, real-time data, and precision planning. One of the most impactful innovations in this space is robot assisted knee surgery, which is redefining how accuracy is achieved in modern joint replacement. This blog explains how robotic knee replacement enhances surgical accuracy, why precision matters so much in knee outcomes, and what patients should realistically expect. Why Surgical Accuracy Matters in Knee Replacement Accuracy in knee replacement is not a technical luxury—it directly affects how long the implant lasts, how natural the knee feels, and how quickly patients recover. When a knee implant is placed even a few millimeters off alignment, it can lead to: Uneven wear of the implant Persistent pain or stiffness Reduced range of motion Early implant failure Need for revision surgery Traditional knee replacement techniques rely heavily on manual alignment tools and visual judgment. While experienced surgeons achieve good results, human estimation still has limitations. This is where robotic assistance changes the game. What Is Robotic Assistance in Knee Surgery? Robotic assistance in knee surgery uses computer-guided technology to help surgeons plan and execute the procedure with extremely high precision. Contrary to common belief, robots do not perform surgery independently. The surgeon remains in full control at every step. The robotic system acts as an intelligent assistant that: Creates a detailed 3D model of the patient’s knee Guides bone cuts within predefined safe boundaries Continuously adjusts to real-time feedback during surgery This combination of surgeon expertise and digital precision is what enhances surgical accuracy beyond what manual techniques alone can achieve. Pre-Surgical Planning: Accuracy Starts Before the First Cut One of the biggest advantages of robotic-assisted knee procedures is what happens before surgery even begins. Personalized 3D Knee Mapping Using advanced imaging and data mapping, the robotic system builds a virtual 3D model of the patient’s knee. This allows the surgeon to: Analyze bone structure, cartilage loss, and deformities Assess ligament balance and joint mechanics Plan implant size and positioning with sub-millimeter accuracy This personalized planning replaces one-size-fits-all approaches and ensures the surgical strategy is tailored to the patient’s anatomy. How Robotics Improve Bone Cutting Precision Bone cuts are the foundation of knee replacement accuracy. Even slight deviations can affect implant alignment and long-term function. Controlled, Guided Bone Resection During surgery, the robotic system provides: Visual guidance on screen Physical boundaries that prevent overcutting Real-time feedback if alignment deviates from the plan This ensures that bone removal is limited strictly to what is necessary—no more, no less. As a result, implant placement becomes more accurate and reproducible. Real-Time Adjustments for Better Alignment Every knee behaves differently once the joint is opened. Ligament tension, soft tissue balance, and joint movement can change during surgery. Robotic systems continuously analyze knee movement through the full range of motion, allowing surgeons to: Adjust implant position instantly Balance ligaments more precisely Optimize knee stability and flexibility This dynamic assessment is nearly impossible to replicate with conventional tools alone. Enhanced Implant Positioning and Longevity Accurate implant positioning is one of the strongest predictors of long-term success in knee replacement. With robotic guidance: Implant angles are optimized Joint alignment is restored closer to natural anatomy Load distribution across the knee becomes more even Clinical studies consistently show that better alignment reduces implant wear, lowers revision risk, and improves patient satisfaction over time. Smaller Errors, Bigger Impact on Recovery Precision doesn’t just affect long-term outcomes—it also influences early recovery. When robotic assistance is used: Less healthy bone is removed Soft tissue damage is minimized Swelling and inflammation are often reduced This can translate into: Faster mobility Better early knee function Shorter hospital stays While recovery still varies by patient, surgical accuracy plays a significant supporting role. Comparing Manual vs Robotic Knee Surgery Accuracy Aspect Manual Knee Surgery Robotic-Assisted Surgery Bone cutting accuracy Surgeon-dependent Computer-guided precision Implant alignment Visual estimation Real-time digital tracking Soft tissue balance Manual assessment Dynamic motion analysis Personalization Limited Highly individualized Reproducibility Variable Consistently high This comparison explains why many centers now consider robotic assistance a major advancement rather than a trend. Does Robotic Accuracy Benefit All Patients? Robotic accuracy can be particularly beneficial for: Patients with knee deformities Younger, active individuals seeking long implant life Patients with complex anatomy Those who want highly personalized surgery However, success still depends on surgeon expertise, proper patient selection, and high-quality post-operative rehabilitation. At advanced centers like Orthomax 3D Knee Institute, technology is combined with experience—not used as a replacement for it. Addressing Common Myths About Robotic Knee Surgery “The robot performs the surgery” False. The surgeon controls every step. The robot only assists. “Robotic surgery is experimental” Not true. Robotic-assisted knee procedures are widely used globally with strong clinical data. “It guarantees pain-free recovery” No surgery can guarantee outcomes, but improved accuracy significantly increases the chances of better results. Is Robotic Surgery the Same as the Best Surgical Outcome? Technology alone does not define the best knee replacement outcome. Accuracy, surgeon skill, implant quality, rehabilitation, and patient commitment all work together. Robotic systems enhance precision, but results still depend on: Correct surgical planning Proper implant selection Structured physiotherapy Long-term lifestyle care When all these factors align, patients experience the most natural-feeling and durable knee outcomes. Cost vs Value: Is Robotic Accuracy Worth It? Robotic-assisted procedures may involve higher upfront costs. However, when evaluated long-term, improved accuracy can mean: Lower revision surgery risk Better functional outcomes Higher patient satisfaction For many patients, this makes robotic assistance a value-based investment rather than an added expense. Future of Surgical Accuracy in Knee Replacement As robotic systems continue to evolve, we can expect: Even more refined personalization AI-driven predictive planning Better integration with patient recovery data Accuracy will increasingly become the standard rather than the exception. FAQs: 1. How does robotic assistance improve surgical accuracy? Robotic systems provide real-time